Degenerative Disc Disease
![]()
Call (703) 520-1031 or use the form to send us your contacts.
Aging can lead to the development of a variety of medical conditions, and degenerative disc disease is one of them. Technically, it is not a disease. It is an age-related condition that develops due to wear and tear on spinal discs over a period of time and may become painful. Injuries and other factors can influence the rate and severity of the natural degeneration process. The following sections provide an overview of the disease, including symptoms, causes and treatments.
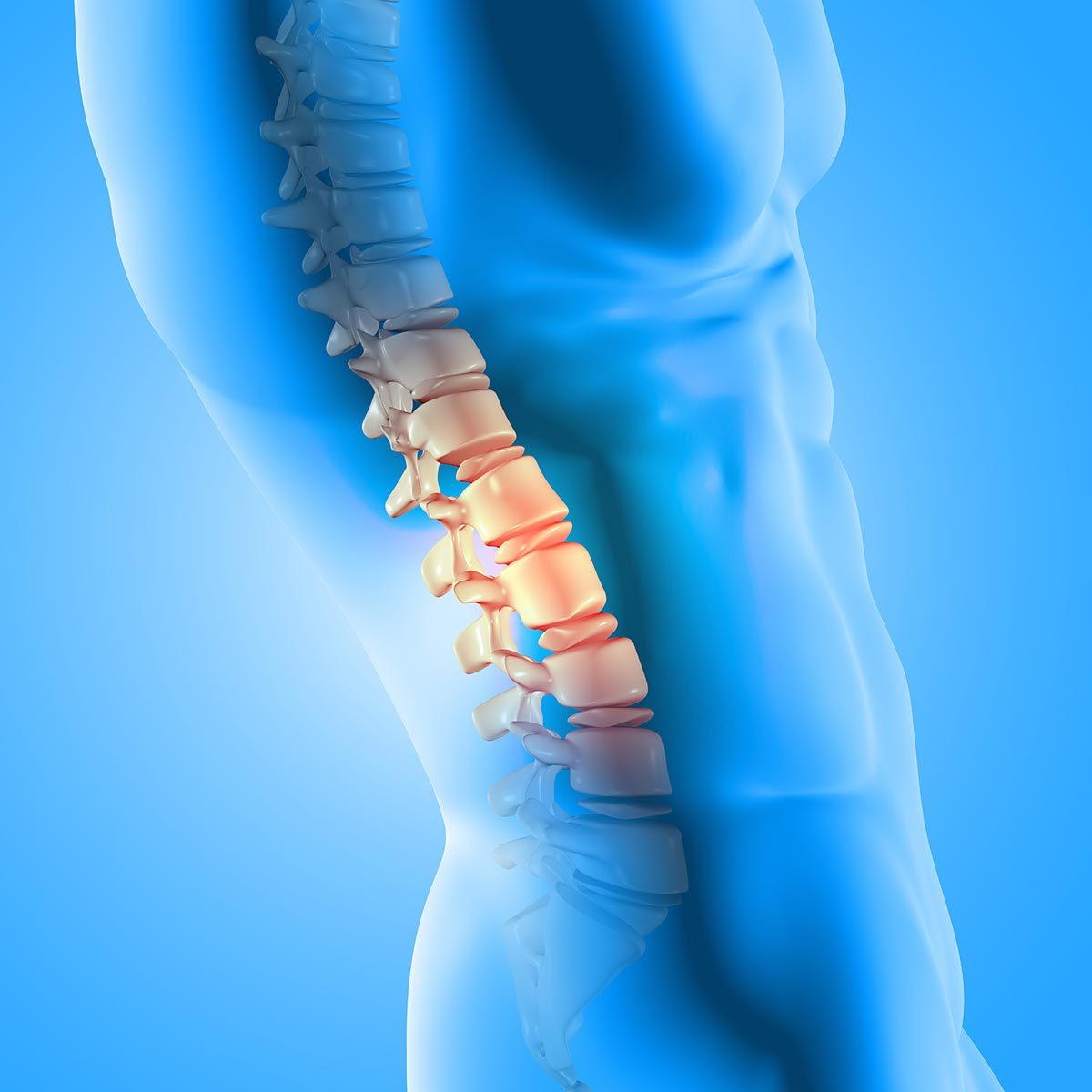
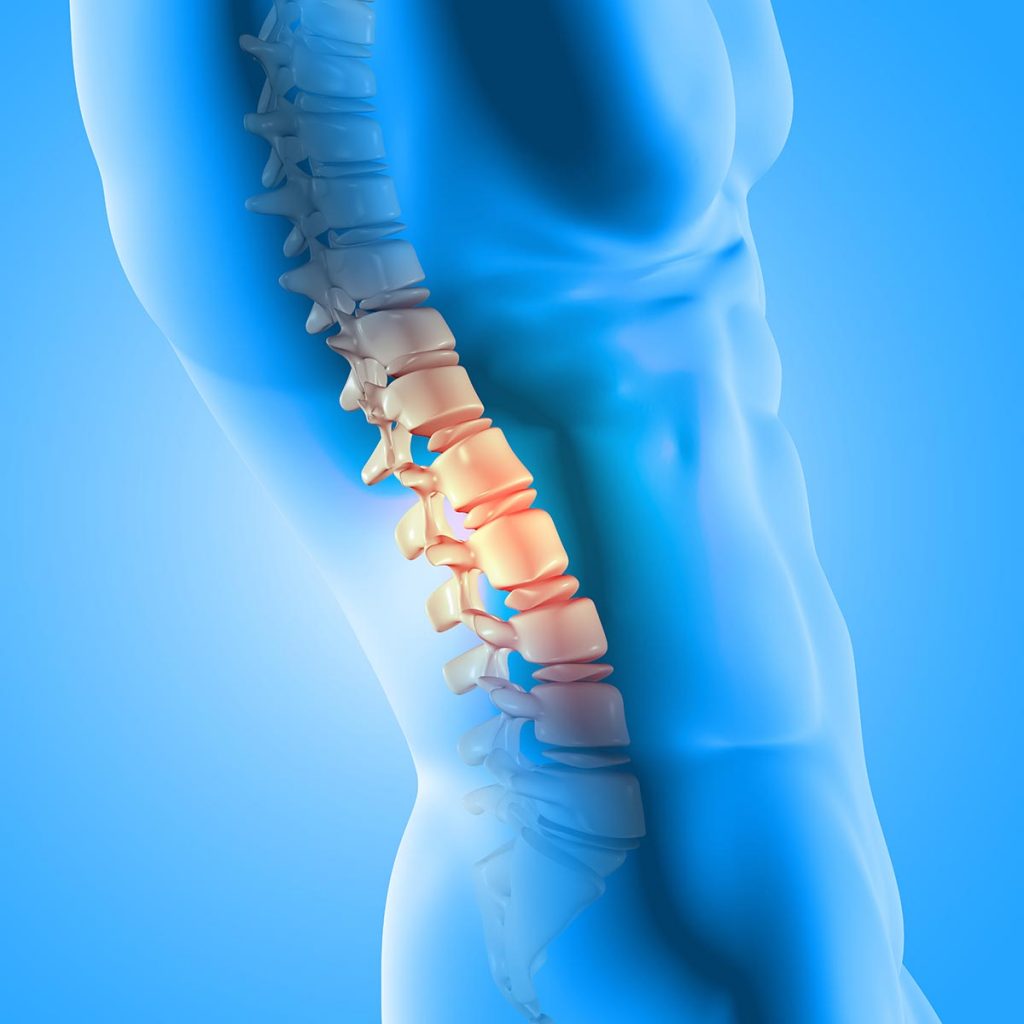
What is Degenerative Disc Disease?
The spinal column has spongey discs between the spinal bones. The discs serve as cushions that absorb the force of movement and pressure placed on the spine. Each disc has two parts. One is the annulus fibrosus, a tough outer layer that contains shallow nerves. The disc interior, called the nucleus pulposus, is best described as a soft, jelly-like substance that is filled with proteins. People experience pain when the outer or inner sections of the disc are damaged or deteriorate, impacting the nerves in and around the spine.
Symptoms
The back is made up of three major sections, called the cervical (neck), thoracic (middle) and lumbar (lower back) areas. When the discs degenerate, the symptoms can vary from person to person. Though any disc can degenerate, most people experience pain or stiffness in the neck or lower back.
Pain, numbness, tingling and weakness are four major symptoms that can occur individually or in some combination when one or more spinal discs deteriorate. Symptoms include the following:
- Pain in the cervical area – Neck pain remains isolated in the neck.
- Radiating pain in the neck area – Pain from degenerative disc disease in neck radiates to the hands and arms.
- Pain in the lower back worsens while sitting – Sitting places significantly more pressure on the lower spine.
- Radiating pain in the lower back, thighs and buttocks – Pain radiates from the lower back into other areas.
- Weakness in leg muscles – Muscles weaken due to damaged nerve roots.
- Pain that varies – Pain can vary in that it may come and go; last a few days or remain unrelenting; worsen during certain movements like twisting and bending; improve during certain movements like walking or changing positions; and range from mild to severe and disabling.
While any spinal disc can deteriorate, lumbar and cervical degenerative disc disease are the most common.
Pain is the most common symptom of disc disease due to degeneration. The causes of pain include:
- A tear in the annulus fibrosis reaches the nerves on the periphery.
- A crack in the annulus fibrosis allows the soft core to bulge and affect nearby nerves or cause a disc to slip out of place.
- The inner section of the disc leaks its inflammatory proteins, and they make contact with a nerve root that becomes inflamed and shoots pain down the leg or armor into the legs.
- The inner section of the disc leaks its inflammatory proteins, and they make contact with the nerves in the annulus fibrosis.
- Loss of water in the disc leads to bones in the spine making contact, irritating surrounding tissues.
- Damaged disc leads to spine instability, which causes painful /muscle spasms as the body attempts to stabilize.
Though most people will develop degenerative disc disease due to again, not everyone experiences pain.
Causes
Though it is called an age-related disease, several possible factors determine the rate and severity of disc deterioration.
1. Age
Spinal discs are 80 percent water at birth, but they dry out over the decades and lose their resiliency.
2. Everyday movements
Repetitive movements, like a lot of lifting, can cause disc wear and tear.
3. Sports
Intense movements can cause tears in the annulus fibrosus.
4. Injuries
Work-related injuries, car accidents, slips and falls at work or home, and participation in athletic activities can damage discs.
5. Genetics
Ongoing studies also explore whether genetics make some people more likely to develop symptomatic disc disease.
6. Lifestyle
Activities like smoking and factors like obesity can accelerate or intensify the normal degenerative process.
Only the outermost layer of spinal discs has blood vessels, so damaged spinal discs cannot repair themselves.
Diagnosis
Degenerative disc disease pain lowers the quality of life and drives people to seek medical attention. The physician will:
- obtain a medical history;
- document a detailed description of the symptoms experienced;
- ask patients to perform certain movements, like twisting and sitting, to pinpoint the problem area;
- check for pain associated with the application of pressure to certain back areas;
- check for indications of muscle weakness;
- check for nerve functioning by testing reflexes and response to hot and cold stimuli.
Conventional X-rays can detect damage in the bones of the spine. However, since discs are soft tissue, imaging scans are necessary. They include an MRI (magnetic resonance imaging) or a CT scan (computed tomography scan). Since most people experience some level of disc degeneration during their lifetime, the scan alone is not enough to determine the source of pain.
Treatment
Non-Surgical Treatments
Surgical treatments are a last resort treatment when non-surgical treatments do not relieve pain. Non-surgical treatments include:
- taking over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen or muscle relaxants;
- taking prescription pain relievers to reduce inflammation and/or relieve muscle spasms;
- getting one or more shots, called facet joint injections, of powerful steroid medication to reduce inflammation and swelling;
- attending physical therapy sessions designed to strengthen supporting muscles from the neck to the lower back;
- doing gentle, low-impact exercises, including walking and stretching, also designed to strengthen back muscles and decompress the spine;
- losing weight and/or quitting smoking;
- getting massages to relieve muscle tension;
- using heat and cold therapy.
Surgical Treatments
The physician will likely recommend a combination of non-surgical treatments. In some cases, surgery is needed when all other treatments fail to reduce the pain or other symptoms after a few months, or the condition becomes a disability. A lumbar or cervical degenerative disc disease disability makes it difficult to work, perform daily activities and enjoy life. There are two basic types of surgeries.
- Minimally invasive surgery
A variety of minimally invasive surgical procedures, including spinal stabilization procedures, do not require large incisions. These include facet thermal ablation, which deadens nerves causing pain, and posterior cervical fusion, which requires only a small incision in the back of the neck to fuse adjacent vertebrae for greater stability.
- Invasive surgery requiring open spine procedures
Open spine surgery is the most invasive type of surgery and is only used in extreme cases. The most common procedure is the open spine fusion, in which two or more vertebrae are permanently fused. A spinal fusion requires large incisions and significant surgical procedures to remove degenerated discs and stabilize the spine with hardware.
Living with chronic pain is debilitating. When back pain interferes with daily activities, it is time to see a spine specialist. There are many options for treatment, so there is no reason to live with pain that has a good chance of responding to treatments.