Table of Contents
Back pain is a common medical problem, affecting as many as 8 out of 10 people in their lifetime, according to research found at the U.S. National Library of Medicine. Research at the U.S. National Institute for Occupational Safety and Health has also shown that almost 40 million U.S. workers are experiencing low back pain.
Facts About Pain
Everyone experiences pain, usually many times in their lifetime. Following are a few facts about pain.
- Pain is experienced on a spectrum and can come and go, depending on the cause of the pain.
- There are three types of pain: nociceptive pain (tissue damage), neuropathic pain (nerve dysfunction or damage), and inflammatory pain (immune system related).
- An estimated 50-plus million U.S. adults are experiencing chronic pain.
- Approximately 20.4% of U.S. adults experience chronic pain and 7.4% experience high-impact chronic pain that limits work or life activities.
- More women than men experience chronic pain (21.7% compared to 19%) and high-impact chronic pain (8.5% to 6.3%).
- Common causes of acute pain include broken bones, strained muscles, surgery and infections.
- Approximately 65 million Americans experience back pain, one of the most frequent complaints doctors hear.
- Approximately 54.4 U.S. adults have arthritis, expected to increase to 78.4 million people by 2040 (6); about 55.3% of adults with diagnosed arthritis experience severe or moderate joint pain.
These facts about pain indicate that over a third of adult Americans are living with pain.
With so many people dealing with back pain, it is not surprising that many myths or misconceptions have developed about causes, impacts and treatments. Following are some of the common “mythconceptions” that are pervasive.
Myths and misconceptions about pain keep individuals from seeing a doctor and learning about the best pain treatment for their particular situation. A doctor can assess the cause of pain and recommend the best course of treatment, which could be home self-care or a more comprehensive doctor-supervised treatment plan. The following are the top common myths and misconceptions about acute and chronic pain.
Common Myths Associated with Pain
#1. Pain is always bad
Pain is not always bad. For example, temporary muscle soreness from exercising is not necessarily bad and is probably where the expression “no pain, no gain” came from. When the soreness is short-term, it means muscles are being built up by microtears in the muscles that heal quickly. Mild muscle pain and soreness can last a few days and should ease. If the pain worsens after a few days, more serious muscle tears or ligament ruptures may have occurred.
#2. Exercise will make back pain worse
One of the misconceptions is that exercise should be avoided because it will make back pain worse. Exercise does not make back pain worse. It helps ease back pain for several reasons.
Exercise stretches muscles, ligaments and tendons that have tightened due to stress or a medical condition. It strengthens muscles in the back and abdomen which helps stabilize the spine and provides additional support for the back. Daily moderate exercise is recommended.

#3. Back pain is the result of injury
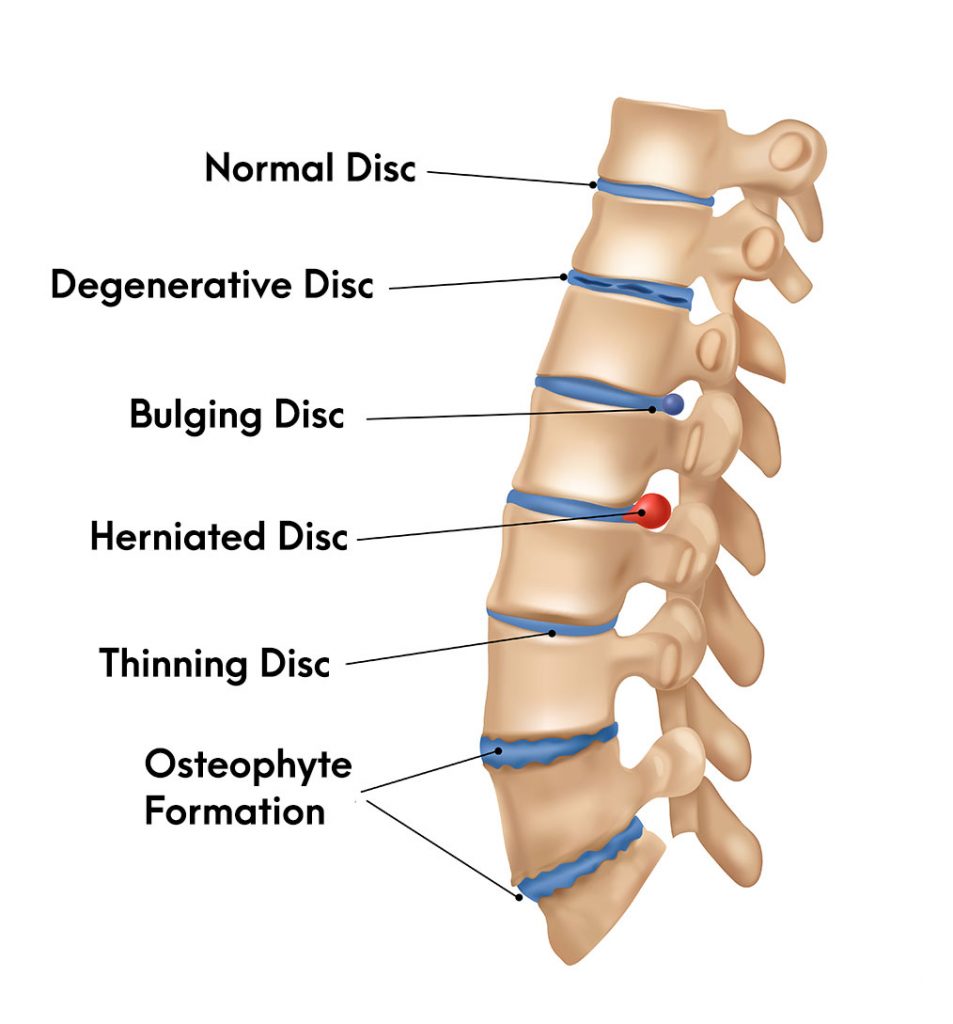
You can experience back pain without injury. There are many reasons a person develops back pain. They include a herniated disc, sciatica, spinal stenosis and arthritis, to name a few. Damaged discs in the lower back, like herniated lumbar discs, are one of the most common causes of lower back pain. A herniated disc can lead to the gel-like material in the disc irritating and inflaming spinal nerves. There are even causes that are not connected to the back structures, like kidney stones and pregnancy.
Pain is a complex experience that may happen for multiple reasons unrelated to injury. For example, headache pain may be due to emotional, behavioral or psychological factors. Headache pain accounts for 3.5% of U.S. patients experiencing chronic pain.
#4. Pain is inevitable during the aging process
One of the myths about chronic pain is that older individuals will have to be stoic and live with debilitating pain. This stereotype of the pain-aging connection is false, leading to people not seeking medical advice and treatment when they would benefit from it. The truth is that chronic pain is not a natural part of aging, and people telling themselves it is something they have to live with does not make pain more tolerable. Seeking medical information on pain management and treatments for example at our Spine and Pain clinic is important to minimizing pain that may impact lifestyle.
#5. Bed rest is good for easing back pain
This could also be named as one of the biggest myths about the pain experienced in the back, especially lower back pain or sciatica. Laying down leads to changes in the back’s structures and alignment that can increase back pain.
For example, research has shown the intervertebral disc increases in size because it absorbs fluids and swells. In addition, laying down changes the curvature of the spine by flattening it. It is one reason people who normally have no back pain issues will complain of back pain after staying in bed too long. Minimizing physical activity to accommodate back pain is not a good strategy, and over the long term will lead to even more issues, like weak muscles.
#6. Stress is not a cause of back pain
Stress may be an emotional experience, but it causes physical responses. Stress leads to changes in breathing that cause tension in back muscles, can cause poor posture due to fatigue and promotes inactivity. It can also lead to tight muscles, especially in the neck.
#7. Severe back pain means there is a serious medical problem
Back pain can range from mild to moderate to severe. It is natural to automatically assume severe back pain or a painful flare-up means something very serious is happening. In some cases, it might be.
For example, back pain may be due to degenerative disc disease that needs intervention. Often the pain is due to something less serious, like a pulled back muscle, and occurs when doing a specific activity, like lifting or twisting. If the pain continues to lessen and goes away over 3-5 days after home treatment, like applying ice, it is unlikely there is a serious medical problem.
#8. Bulging spinal discs are always a major medical issue
Bulging discs commonly develop as people age. A bulging disc may or may not cause back pain. It may cause pain when it places pressure on nearby nerves, but the bulging disc can often be treated with anti-inflammatory medications, application of heating pads and light exercise. Bulging discs become a serious problem when there is severe pain indicating the disc is near herniation or the pressure on nerves creates issues like numbness or weakness in a leg or loss of bladder control.
#9. Spine surgeons always recommend surgery to relieve back pain
Spine surgeons do not always recommend surgery to treat chronic spine pain. In fact, spine surgeons will always first develop non-surgical treatment plans. Most back pain problems are resolved without surgery. Even if you are living with chronic back pain, the first treatment options are non-surgical, but it does take adherence to the treatment plan your doctor recommends.
#10. Pain management always requires addictive pain medications
This is not true. One of the common myths about pain management is that potentially addictive opioids are usually prescribed, especially for chronic pain, but there are many other alternative treatment types. They include nonsteroidal medications (OTC), physical therapy, exercise and lifestyle changes like losing weight and improving diet. Sometimes, a minor medical procedure targeting the cause of pain is all necessary, and the OTC medications are strong enough.
Myths Cause Confusion
People experience pain in many different ways, which is one reason myths about pain management exist. It is essential to pay attention to pain and not try to ignore it, whether acute or chronic. Home treatments often ease acute pain, but a pain specialist should assess any pain lasting more than a few days. Pain doctors at our clinic can diagnose the source of pain and offer various solutions to fit a patient’s specific needs.
Sources
- https://medlineplus.gov/backpain.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6611834/
- https://www.cdc.gov/acute-pain/low-back-pain/index.html
- https://www.webmd.com/back-pain/news/20190513/1-in-4-american-workers-struggles-with-back-pain
- Fernandez M, Hartvigsen J, Ferreira ML, et al. Advice to Stay Active or Structured Exercise in the Management of Sciatica. Spine. 2015;40(18):1457-1466. PMID: 26165218 doi:10.1097/brs.0000000000001036
- Belavý DL, Armbrecht G, Richardson CA, Felsenberg D, Hides JA. Muscle Atrophy and Changes in Spinal Morphology. Spine. 2011;36(2):137-145. doi:10.1097/brs.0b013e3181cc93e8
- Alturkistani LH, Hendi OM, Bajaber AS, et al. Prevalence of Lower Back Pain and its Relation to Stress Among Medical Students in Taif University, Saudi Arabia. Int J Prev Med. 2020;11:35. Published 2020 Mar 16. doi:10.4103/ijpvm.IJPVM_264_19
